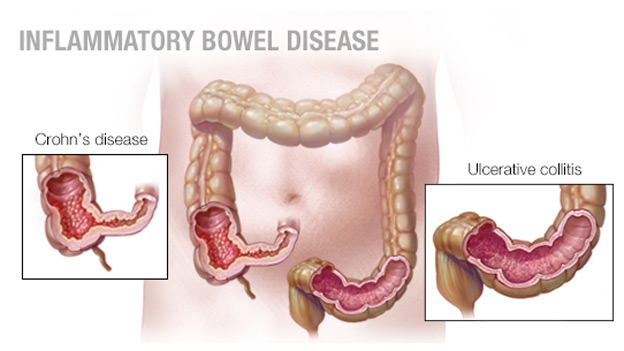
The death rate for Crohn’s disease is quite low. The most common cause of increased mortality associated with CD is the development of malignant gastrointestinal tumors, including cancer of the colon and small intestine.
Pathophysiology: Ulcerative colitis usually begins with a lesion of the rectum. The process may remain localized at this level (ulcerative proctitis) or spread in the proximal direction, in some cases the entire colon is affected. In rare cases, colitis from the outset covers most of the colon. Inflammation in the framework of UC affects the mucous membrane and submucosal layer, characterized by a clear boundary between healthy and diseased tissue. The muscular layer is affected only with severe course. In the early stages of the disease, the mucous membrane is erythematous, the surface is covered with small granules, easily vulnerable, the normal vascular pattern disappears, and scattered hemorrhagic elements are often identified. Severe forms are characterized by large ulcerations of the mucosa with copious purulent discharge. Islets with respect to intact or inflamed hyperplastic mucosa (pseudopolyps) project above the ulcerated surface. Formation of fistulas and abscesses in this case usually is not observed.
Forecast: As a rule, ulcerative colitis has a chronic course with alternating exacerbations and remissions. In about 10% of cases, the first attack proceeds with lightning speed, with massive blood loss, perforation, sepsis and toxemia. In the other 10% of patients after a single attack, there is a complete recovery.
With limited ulcerative proctitis, the prognosis will be the better. The probability of pronounced systemic manifestations, the development of complications associated with toxemia, and malignant degeneration is small, and the increase in the prevalence of the process at a later time is observed only in 20-30% of cases. Surgical treatment is rarely required, life expectancy is not different from the norm. In some cases, symptoms may persist and not respond to treatment. Extensive forms of ulcerative colitis can manifest from an isolated lesion of the rectum, and then spread proximally, so proctitis can be considered localized only after ≥ 6 months of the disease. Localized forms that become common in the future tend to be more severe and are more resistant to treatment. Approximately one-third of patients with extensive ulcerative colitis need surgical intervention. Colon cancer: The risk of colon cancer is clearly associated with the duration of ulcerative colitis and the extent of the lesion, but there is no clear dependence on the clinical severity of exacerbations.